What Are The Difficulties Faced in EMS services?
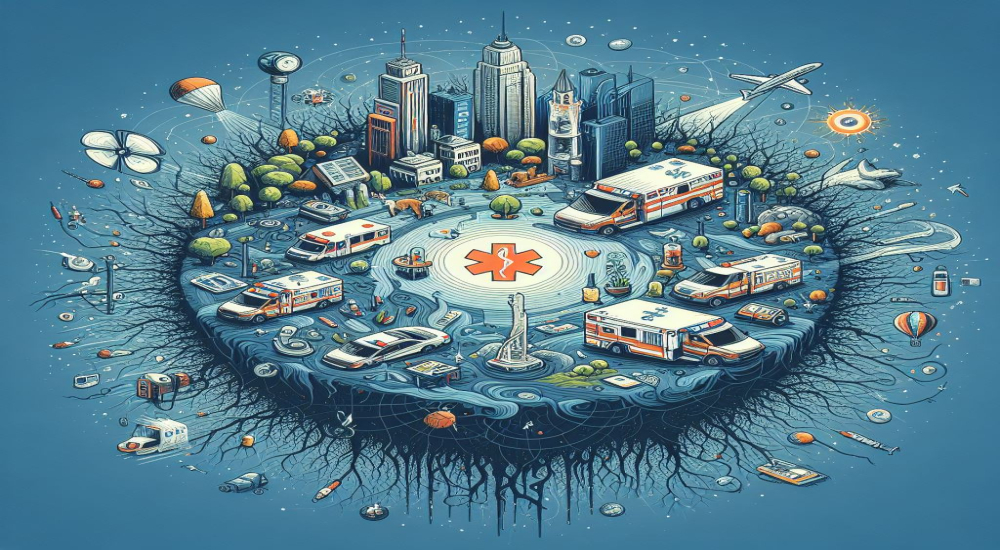
1. PATIENTS ARE THE FOUNDATION
The process of developing and initiating a new, urban EMS system from the ground up in a matter of months isa herculean task to say the least. When establishing an EMS service there are regulations and laws to adhere to at both the state and national level.
2. ERRORS OF THE MIND VS. ERRORS OF THE HEART
One of the most common medical director questions is, “Can I be fired for a clinical mistake?” and the answer at ESD11 Mobile Healthcare is, absolutely not. However, clinical errors of the mind will inevitably occur.
Prehospital medicine is the culmination of thousands of split-second decisions made with limited information. There is always more to learn and areas for remediation. The clinical department and medical director exist primarily to support, educate and guide the field medics so that they can care for patients at the highest level possible.
Errors of the heart, such as lying, fraud, racism and neglect, are much more difficult to fix, yet easier to manage.
3. ASSUME PATIENTS ARE SICK
Throughout various emergency care venues, whether EMS or emergency department, it is not uncommon to see the dangerous attitude creep in where patients must prove to the providers that their illness or complaint reaches some ill-defined “emergency” standard.
Paramedics are triage experts in EMS, which is an underappreciated skill, to say the least. To triage properly, however, providers must operate under the assumption that every patient has an emergency and it’s up to us in EMS to not miss it. This doesn’t mean every patient gets intubated and defibrillated, but it does mean that every patient gets a thorough and efficient exam, with full vitals, a differential consisting of the possible killer diagnoses and rapid transport to the most appropriate resources. We are in the business of death and disability, not of minimization.
4. IN CHARGE MEANS IN CHARGE
At Harris County ESD11 Mobile Healthcare, we operate under a hierarchy of paramedic credentialing. The in-charge paramedic is the lead on each ambulance and the backbone of all clinical care.
The concept of paramedic consultation with supervisors and online/offline medical direction exists in a variety of forms throughout EMS. It is our belief that if we train our most qualified providers to wear the title of “in-charge,” then our protocols and practices should allow them to be in clinical command on scene. This allows for the quickest care and transport decisions for our patients. There are occasional checklist verification and supervisory consultation situations, but these are few and far between.
5. BUT … LIFELINES EXIST
There are certain times when supervisor and medical director support and input are needed. A prime example is high-risk/difficult patient refusals of transport. These situations are tough for all emergency providers.
Sometimes, patients change their minds in situations where we feel they are sick and we’re unsure that they can comprehend the consequences. What’s our end goal? To get our patients to the correct resources promptly. Anecdotes and evidence tell us, a push from the supervisor or urging from the medical director can encourage our patients to make safe decisions. No paramedic will be left on an island in our service.
6. WHEN WE SAY TIME SENSITIVE, WE MEAN IT
There are certain patients and diagnoses where we can positively affect outcomes based on proper scene management and transport decisions (not to get into the details of which time metrics are more valid than others). Large vessel occlusion strokes do better with earlier endovascular retrieval. Trauma patients have better outcomes with shorter on-scene times. EMS recognition of STEMI leads to quicker revascularization.
These facts are not news to anyone reading this, but they do form the foundation of QI/QA metrics and KPIs within any high functioning EMS system. Paramedics must know clear expectations before they can ever be expected to reach any metric goal.
7. TRANSPARENCY IS KEY
Forming a transparent foundation for QA/QI is key as this is the initial source of data within any EMS clinical department. Patient outcomes will be the basis of all continuing education, quality initiatives and protocol revisions for ESD11 Mobile Healthcare. This includes not only EMS outcomes, but also a robust system of data exchange with our hospital partners as well. We are a tax supported, third-service EMS system, so these transparent metrics, KPIs and educational initiatives will always be publicly available to the paramedics, receiving institutions and citizens of the district.
8. EVIDENCE BASED (FOR PATIENT’S SAKE)
Many paramedics inquired about progressive protocols during their initial interview process. We will be progressive at ESD11 Mobile Healthcare, but it will absolutely be progressive for patient’s sake. The newest bell or shiny object are always desired across emergency care. Protocol updates, pharmacologic additions and procedural advancements will only be initiated if the service feels a gap in current patient care can be filled with the change. If said change is made, then open and transparent data collection will take place with an end goal and plan in place, for eventual peer-reviewed validation. This is the full circle of EMS clinical transparency.
9. WITH PARALYSIS AND RESTRAINT COME GREAT RESPONSIBILITY
Spider Man popularized the quote, “With great power comes great responsibility.” This applies directly to any progressive or advanced EMS service capable of paralytic assisted intubation and/or chemical restraint. Pharmacologic and procedural detail aside, we must consider and always respect the gravity of taking over the faculties of a fellow human to better breathe or care for them.
This is a monumental decision that is accompanied by the absolute, non-negotiable requirement that paramedics and emergency providers know associated protocols with medication dosages, indications, contraindications and side-effects. The gravity and importance of airway management and chemical restraint was the focus of all clinical education that followed our 10 clinical commandments discussion.
0. KINDNESS IS EXPECTED
The Mobile Healthcare clinical 10 commandments start and end with the patient as our foundation. We must always put the patient first. In addition, kindness, compassion and empathy are expected.
As first responders, we have the honour of meeting our public on their worst days. Heart attacks, strokes and motor vehicle crashes are often the most emotionally and physically traumatic days of those individual patient’s lives. Yes, we see these events shift after shift, but we cannot underestimate our ability to have positive (or negative) impact on each patient that they will forever remember.
A mentor and giant of emergency medicine, Dr. Kevin Rodgers, often said, “Patients don’t care how much you know until they know how much you care.”