Addressing Maternal Mortality in India: The Role of Telemedicine and Remote Monitoring
Introduction:
Maternal mortality remains a significant public health concern in India, despite considerable advancements in healthcare. The country continues to grapple with high rates of maternal deaths, largely attributed to a combination of health issues and infrastructural challenges. However, innovative solutions leveraging technology, such as mobile-based telemedicine and remote monitoring applications, hold promise in mitigating these challenges and improving maternal healthcare outcomes.
The Maternal Health Landscape in India
India's maternal mortality rate (MMR) reflects the stark reality of healthcare disparities and systemic challenges. According to the World Health Organization (WHO), India accounted for approximately 17% of global maternal deaths in 2017. Despite notable progress in reducing maternal mortality over the past few decades, the rate of decline has been uneven across regions and socioeconomic strata.
Several factors contribute to the persistently high MMR in India:
1. Health Issues: Maternal mortality often stems from preventable or treatable complications related to pregnancy and childbirth, such as severe bleeding, infections, high blood pressure, and unsafe abortions. Limited access to quality maternal healthcare services exacerbates the risk of complications, particularly in rural and under served areas.
2. Lack of Infrastructure: Inadequate healthcare infrastructure, including shortages of skilled healthcare providers, medical equipment, and facilities, poses significant barriers to accessing timely and appropriate maternal care. Remote and rural areas face acute shortages of obstetricians, gynecologists, and trained birth attendants, leading to delays in emergency obstetric interventions and increased maternal morbidity and mortality.
3. Socioeconomic Factors: Socioeconomic disparities play a crucial role in maternal health outcomes. Women from marginalized communities, including those belonging to low-income households, rural areas, and ethnic minorities, often face barriers such as limited education, financial constraints, cultural norms, and social stigmas, which impede their access to maternal healthcare services.
The Potential of Telemedicine and Remote Monitoring
Telemedicine, defined as the remote diagnosis and treatment of patients using telecommunications technology, presents a promising solution to bridge the gaps in maternal healthcare delivery in India. By leveraging mobile-based telemedicine platforms and remote monitoring applications, healthcare providers can extend their reach to underserved populations, facilitate timely interventions, and improve maternal health outcomes.
1. Enhanced Access to Care: Telemedicine platforms enable pregnant women, especially those residing in remote or rural areas with limited access to healthcare facilities, to connect with qualified healthcare professionals virtually. Through video consultations, telemedicine providers can offer prenatal care, conduct routine check-ups, and address maternal health concerns, thereby reducing the need for physical travel and overcoming geographical barriers.
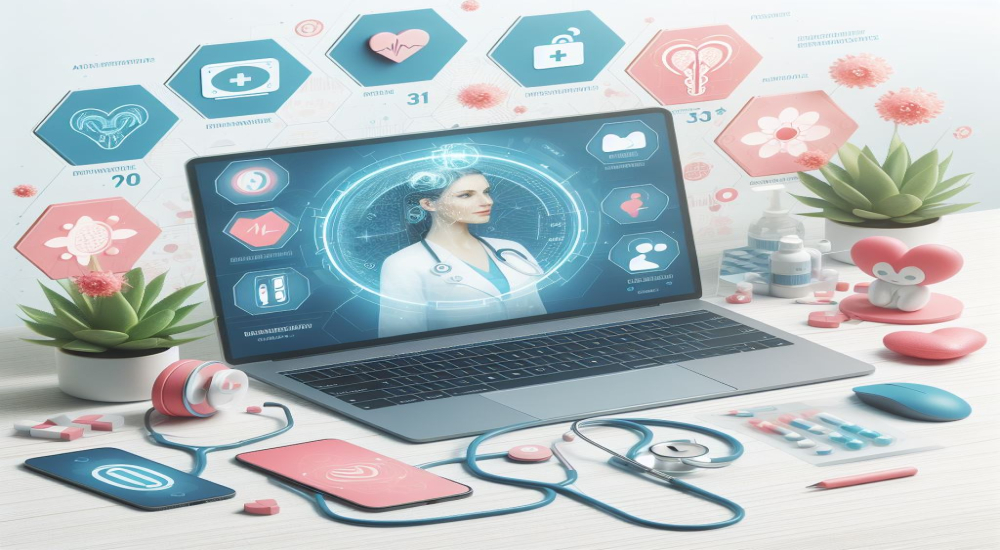
2. Timely Diagnosis and Intervention: Remote monitoring applications equipped with sensors and wearable devices allow healthcare providers to remotely monitor vital parameters and track maternal health indicators in real-time. By detecting potential complications early, such as hypertension, gestational diabetes, or fetal distress, healthcare teams can intervene promptly, initiate appropriate treatments, and prevent adverse outcomes for both the mother and the baby.
3. Automatic Red Flagging of Abnormal Vitals: Incorporating algorithms into remote monitoring applications allows for the automatic detection and flagging of abnormal vital signs, such as hemoglobin levels, blood pressure, weight, and blood sugar levels. When these parameters deviate from normal ranges, the system can generate alerts, prompting healthcare providers to intervene promptly. This proactive approach enables early detection of complications, facilitates timely medical interventions, and reduces the risk of maternal morbidity and mortality.
4. Educational Resources and Support: Mobile-based telemedicine platforms can serve as valuable educational tools, providing pregnant women and their families with access to evidence-based information, prenatal care guidelines, and preventive measures. Through multimedia content, interactive modules, and personalized support, telemedicine applications empower women to make informed decisions about their health, adopt healthy behaviors, and seek timely medical assistance when needed.
5. Continuity of Care: Telemedicine facilitates continuity of care throughout the maternal healthcare continuum, from prenatal consultations and antenatal monitoring to labor and postpartum follow-up. By establishing virtual care networks and coordinated referral systems, healthcare providers can ensure seamless transitions between primary, secondary, and tertiary levels of care, thereby improving care coordination and reducing the risk of medical errors or delays in treatment.
Challenges and Considerations
While telemedicine holds immense potential to revolutionize maternal healthcare delivery in India, several challenges and considerations must be addressed to ensure its effective implementation and scalability:
1. Digital Divide: Disparities in access to digital technology, internet connectivity, and smartphone ownership persist, particularly among marginalized populations and rural communities. Efforts to promote digital literacy, expand internet infrastructure, and provide affordable mobile devices are essential to bridge the digital divide and ensure equitable access to telemedicine services.
2. Regulatory Framework: Clear guidelines and regulatory frameworks are needed to govern the practice of telemedicine, protect patient privacy and confidentiality, ensure the quality and safety of virtual consultations, and establish standards for reimbursement and liability. Collaboration between policymakers, healthcare regulators, and technology developers is crucial to develop robust regulatory frameworks that support innovation while safeguarding patient rights and safety.
3. Healthcare Infrastructure: Telemedicine initiatives must be integrated into existing healthcare systems and complemented by investments in physical infrastructure, human resources, and medical supplies. Strengthening primary healthcare infrastructure, training healthcare providers in telemedicine skills, and equipping facilities with essential telemedicine equipment are essential prerequisites for sustainable telemedicine implementation.
4. Cultural and Social Context: Cultural beliefs, social norms, and community dynamics influence the acceptance and adoption of telemedicine services. Tailoring telemedicine interventions to local cultural contexts, languages, and preferences, engaging community leaders and stakeholders, and fostering trust and rapport with end-users are critical strategies to promote acceptance and utilization of telemedicine among pregnant women and their families.
Conclusion
Addressing maternal mortality in India requires a multifaceted approach that combines clinical interventions, health system strengthening, and innovative technologies. Telemedicine and remote monitoring applications offer a powerful solution to overcome barriers to maternal healthcare access, enhance care quality, and improve health outcomes for mothers and their newborns. By harnessing the potential of telemedicine, India can accelerate progress towards achieving its maternal health goals and ensuring the well-being of its population.
Innovations in telemedicine represent a paradigm shift in healthcare delivery, empowering individuals to access timely and affordable healthcare services, irrespective of geographical constraints or socioeconomic status. As India continues to navigate the complex landscape of maternal health, integrating telemedicine into mainstream healthcare delivery models holds the promise of a brighter, healthier future for mothers and their children across the nation. Automatic red flagging of abnormal vitals adds an extra layer of proactive care, enabling early detection and intervention, ultimately contributing to the reduction of maternal mortality rates in India.