Tele-Ophthalmology: The Vision Of The Future
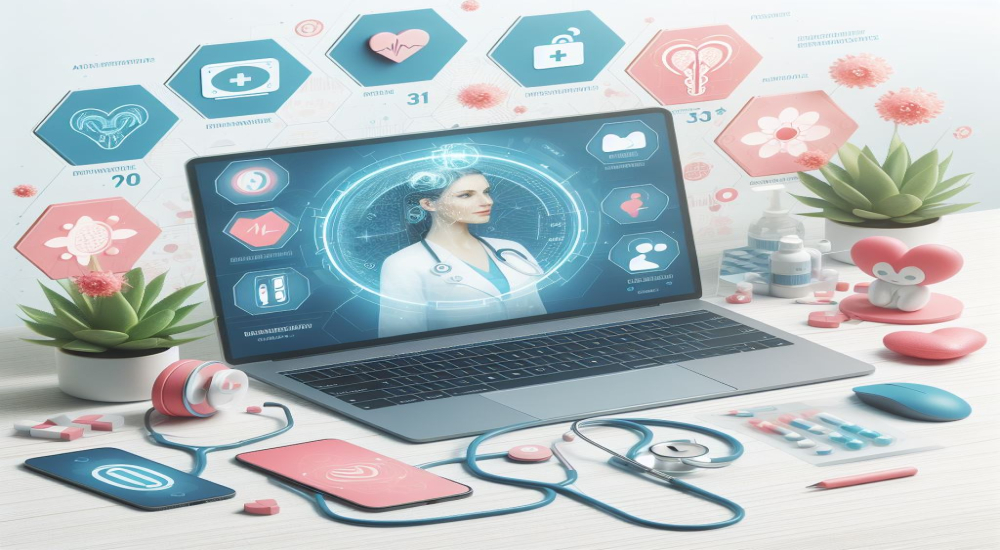
In the vast landscape of modern healthcare, the integration of technology has brought about remarkable advancements, fundamentally altering the way medical services are accessed and delivered. Among the myriad applications of technology in healthcare, telemedicine stands out as a particularly transformative force, offering remote clinical services through the utilization of telecommunications technology. Within this realm, tele-ophthalmology emerges as a beacon of hope, promising to revolutionize the field of eye care by leveraging digital platforms to overcome barriers to access, enhance efficiency, and reduce costs.
Challenges
The landscape of eye care is marked by unique challenges, including disparities in access to specialized services, particularly in remote or underserved regions. Tele-ophthalmology addresses these challenges head-on by facilitating remote consultations, examinations, and management of eye conditions through the use of digital communication tools. At its core, tele-ophthalmology aims to democratize access to eye care, ensuring that individuals, regardless of their geographical location or socioeconomic status, have the opportunity to receive timely and quality eye care services.
Accessibility lies at the heart of tele-ophthalmology's promise. In many parts of the world, accessing specialized eye care services can be a daunting task, with long travel distances, limited transportation options, and scarce healthcare infrastructure presenting significant barriers. For individuals residing in rural or remote areas, seeking ophthalmic care often entails traveling long distances to urban centers where specialists are concentrated. This journey can be prohibitively expensive and time-consuming, deterring many from seeking the care they need. Tele-ophthalmology transcends these geographical barriers by bringing the expertise of ophthalmologists directly to patients' homes through virtual consultations and remote diagnostic imaging.
How Can It Help?
Furthermore, tele-ophthalmology enhances the efficiency of eye care delivery by optimizing the utilization of healthcare resources and reducing wait times for appointments. Traditional in-person consultations often involve lengthy wait times for appointments, leading to delays in diagnosis and treatment initiation. With tele-ophthalmology, patients can connect with ophthalmologists remotely, minimizing wait times and streamlining the care delivery process. Digital imaging technologies allow for the rapid capture and transmission of ocular images, enabling ophthalmologists to assess eye conditions remotely and formulate treatment plans efficiently.
The cost-effectiveness of tele-ophthalmology is another compelling aspect of its implementation. By reducing the need for frequent in-person visits and minimizing travel-related expenses, tele-ophthalmology offers potential cost savings for both patients and healthcare providers. Moreover, early detection and intervention facilitated by tele-ophthalmology can prevent costly complications associated with advanced eye diseases, ultimately reducing the economic burden on healthcare systems. In resource-limited settings, where healthcare resources are scarce and financial constraints are prevalent, tele-ophthalmology presents a cost-effective solution for expanding access to eye care services.
Implementation
Tele-ophthalmology encompasses a wide range of applications across various subspecialties within ophthalmology, each addressing specific clinical needs and populations. One notable application is the use of telemedicine for diabetic retinopathy screening, a leading cause of blindness worldwide. Through remote screening programs, individuals with diabetes can undergo retinal imaging locally, with images transmitted to ophthalmologists for interpretation and triage. This approach enables the early detection and management of diabetic retinopathy, thereby reducing the risk of vision loss and blindness in diabetic patients.
Similarly, tele-ophthalmology has been instrumental in the management of glaucoma, a chronic eye condition characterized by progressive optic nerve damage. Remote monitoring devices allow patients to measure their intraocular pressure and transmit data to healthcare providers for review, enabling timely adjustments to treatment regimens and improved disease management. In pediatric ophthalmology, telemedicine consultations enable pediatricians and primary care providers to seek expert guidance from ophthalmologists regarding the diagnosis and management of pediatric eye conditions, ensuring timely intervention and appropriate referrals when needed.
Furthermore, tele-ophthalmology plays a crucial role in low vision rehabilitation, empowering individuals with visual impairment to optimize their remaining vision and enhance their quality of life. Through tele-rehabilitation programs, individuals receive personalized vision rehabilitation services remotely, including orientation and mobility training, adaptive technology instruction, and psychosocial support. These programs enable individuals with visual impairment to access specialized services from the comfort of their homes, reducing barriers to care and fostering independence and self-confidence.
Hurdles and Pitfalls
Despite its immense potential, tele-ophthalmology faces several challenges and considerations that must be addressed to realize its full impact. Ensuring patient privacy and data security is paramount, particularly given the sensitive nature of medical information exchanged during remote consultations. Robust cybersecurity measures must be implemented to safeguard patient confidentiality and protect against data breaches. Additionally, maintaining the quality of remote consultations is essential to ensure accurate diagnosis and appropriate management of eye conditions. Ongoing training and education for healthcare providers in tele-ophthalmology best practices are essential to uphold standards of care and clinical excellence.
Moreover, addressing technological barriers for elderly or technologically disadvantaged populations is crucial to ensure equitable access to tele-ophthalmology services. User-friendly interfaces, intuitive digital platforms, and adequate technical support are essential to overcoming barriers to adoption and ensuring that all individuals can benefit from tele-ophthalmology. Furthermore, regulatory and reimbursement frameworks must evolve to support the integration of tele-ophthalmology into mainstream healthcare delivery. Clear guidelines and reimbursement policies are needed to incentivize healthcare providers to adopt tele-ophthalmology practices and ensure sustainable funding for tele-ophthalmology initiatives.
Conclusion
In conclusion, tele-ophthalmology holds immense promise as a transformative force in eye care, offering a comprehensive solution to the challenges of accessibility, efficiency, and cost-effectiveness. By leveraging remote technology to overcome geographical barriers, enhance efficiency, and reduce costs, tele-ophthalmology has the potential to revolutionize the delivery of eye care services and improve patient outcomes on a global scale. As technological advancements continue to evolve and healthcare systems embrace digital innovation, tele-ophthalmology is poised to play an increasingly significant role in shaping the future of eye care, ensuring that the gift of sight reaches all who need it, regardless of where they are located or their socioeconomic status.