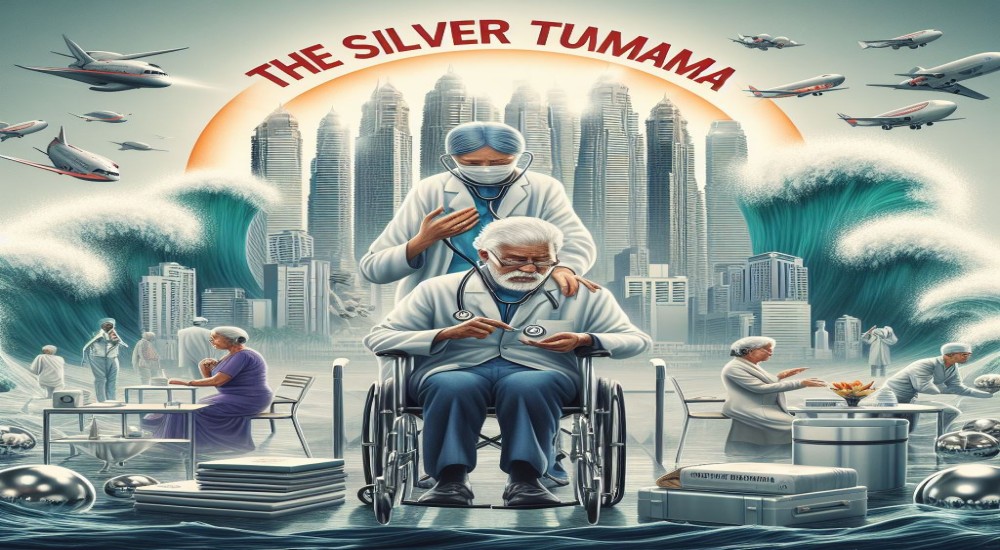
All of us have had the experience of going to the doctor at one point in time or another (unless you're like Wolverine and have a healing factor that keeps you healthy). Depending on the country or city that you are in, your experience with the healthcare system can vary widely. In countries like Canada with a social welfare healthcare system, the treatments are usually of a high standard and free but involve long waiting times and backed-up patient appointments. On the other hand in developing countries with skewed or poor medical infrastructure, the access to professional medical help can be lacklustre and sporadic.
The Friendly Neighborhood Doctor!
All of us have seen, read, or at least heard of the stereotypical neighbourhood doctor. In times when medical facilities were just developing and doctors themselves were in even shorter supply than they are today, we had medical professionals who catered to the communities around their place of residence. Many old movies have a doctor with a big black bag and a stethoscope around his neck as the village or town medicine man, such a site evokes strong nostalgia in many of our parents and older relatives. The main allure was that this village doctor was part of the community he served, had intimate knowledge about the habits and illnesses of the people he treated and was trusted to deliver quality medical care right to your doorstep. In many cases, this doctor would be more trusted by the populace than the "fancy town doctors".
This was a good and sustainable model that helped to address the inequality in access to healthcare in remote locations, in fact, many western countries such as Canada are offering doctors/dentists incentives to settle down and practice in the more remote regions of their countries. This way both the community and the doctor are well served. At least that was the idea, this approach has its own set of pitfalls and shortcomings. Today's medicine has advanced by leaps and bounds and people have also adapted to a higher standard o living that is backed by technology. In such a scenario where a community has diverse medical needs, the community doctor model is not enough.
WHOM WOULD YOU GO TO?
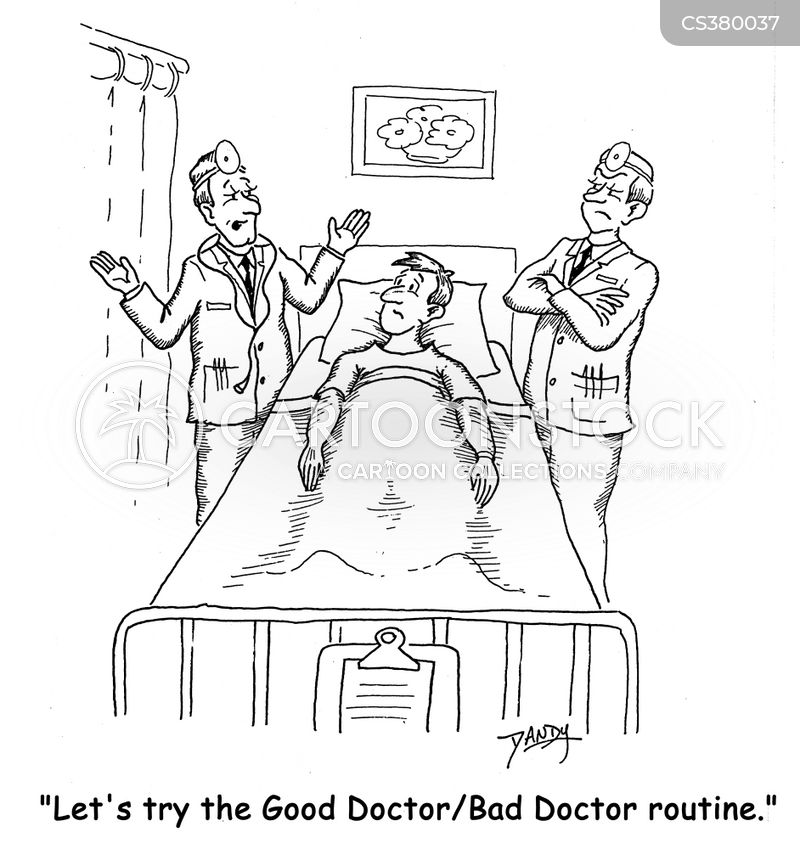
We all have experienced the two broad stereotypes of doctors, in fact, we might have been treated by both types during our lifetimes. The first type is the doctor who listens to your complaint and sends you off to do a variety of diagnostic tests, labs, imaging, etc and then prescribes a bunch of medications that you must take and then sends you off. The second kind is the one that advises you to exercise more, eat healthily, cut down on fatty foods, and basically try out lifestyle changes before taking medications. Now as you are reading this most of you will lean towards one or the other kind of doctor, for most of you, I'll hazard a guess that the doctor who prescribed a bunch of tests and meds is the one you prefer to bet on.
The reason for this is very simple, we might grumble and complain about how the pharma industry works hand in hand with doctors to push more drugs onto the people, but at the end of the day, many of us do believe that medications work and whether they actually do or it's just a placebo effect, we do feel better after taking them.
GETTING YOUR MONEY'S WORTH
For many of us, paying a large consulting fee for a doctor comes with certain expectations on how we will be treated. The doctor who prescribes tests and medications is someone who seems worth the money and the time we spent, contrast that with the physician who told us to simply change the way we live. On the surface and at a certain subconscious level he doesn't seem to be doing justice to the money we paid him. Right?
But the truth is never so simple. Many medical professionals follow a protocol of aggressive testing and heavy prescribing because many of them feel that their patients expect that from them. In the internet age, many doctors and even hospitals are afraid of negative reviews, bad publicity and that dreaded 1-star rating from their patients. In such a climate they often pander to what they see as the patient's needs, even though the proper medical and ethical thing to do would be to do a more detailed examination and advise lifestyle changes before taking the express train to medication city.
One of the things that have come under increasing scrutiny in recent days is which procedures/medications are being prescribed routinely and whether are they actually improving the health outcomes of patients. To the surprise of many people and most importantly doctors themselves, many commonly prescribed treatments were found to have no bearing on the long-term health and survival of patients. An in-depth examination of current medical practices was reviewed and an article was published in the Atlanta magazine (It's a long read but believe me its worth it), the article shed some light on the way certain procedures and medicines continue to be prescribed even though there is no significant scientific evidence that supports their use.
In a country like India where a significant portion of the population is illiterate, and even the highly educated parts of the population can be medically illiterate, there is even greater respect for the doctor who writes you a prescription full of hard-to-pronounce medications. We tend to see a doctor who takes our money and just talks about diet and exercise or lifestyle changes as a doctor without much knowledge or as a slacker who doesn't know what they're doing. There are many calls by various organizations in India that are saying that drug resistance will be the next devastating epidemic to hit our populations. Poor regulatory oversight and an abundance of people who self-prescribe antibiotics and painkillers to themselves or their loved ones have led to the overuse and over-prescription of medicines for conditions that are not even treated by them.
A HARD PILL TO SWALLOW
Recent studies have shown that there is no demonstrable advantage that is seen in prescribing blood pressure medications for preventing heart disease, multiple studies have shown that they do not appreciably decrease the incidence of heart disease. The same could be said for procedures such as stenting in the case of stable anginas, prescribing antibiotics for a variety of conditions, etc. Then why is it that doctors continue to prescribe these medications?
The answer can be two-part: The first one is that doctors feel a certain pressure to perform, patients today are far more well-informed and knowledgeable thanks to the internet, as such doctors who are prescribing medications and tests tend to get ranked higher and get better reviews. In a world of Yelp for doctors, where their ratings and reviews by patients matter, doctors start to follow the trend of prescribing or doing what the patient is most likely to appreciate or look forward to. This can be a fatal loop with both doctors and patients negatively reinforcing unmedical and non-evidence-based decisions in each other.
The other part of the answer lies in the fact that doctors themselves follow certain treatment protocols or prescription patterns because that is what they were taught, it is the same thing that they were trained to repeat over and over by their superiors, guides and professors, even if the current science has relegated that particular treatment method to the garbage pile. Many doctors and even specialists don't really keep up to date with the latest technology, publications and recent advancements in the field of medicine (let's face it, there are 1000s of articles published and redacted each year, so it can be quite overwhelming to keep up with all of them). Just like any other professional group, it's hard to get everyone to agree on one gold standard when it comes to treatments, especially as the patients themselves are so diverse in their medical and physiological makeup.
So a culture of placing billing and rating above patient needs as well as a lack of systematic updates on the latest medical news, developments and discoveries coupled with mismatched expectations from patients on how their doctor should behave or treat them medically all combine together into a recipe for disaster.
PERSONAL MEDICINE VS PROFESSIONAL MEDICINE
This problem is far more than doctors vs patients or old treatment methods vs new ones, it's a more widespread issue that is symbolic of a global healthcare system that is stagnating on the one hand, while also trying to push the boundaries of what's possible on the other. The issue is that medicine today has moved beyond the personal doctor who coasted by on his reputation or his excellent skills, it is now an organized industry where profits and losses are a huge motivator and we cannot pretend otherwise. The practice of personalized medicine depended entirely on the skill and technical soundness of the doctor involved and their reputation in the community. This approach can be troublesome as it has no organizational backing and does not pay attention to protocol.
We need to see a shift from this kind of medical practice that glorified an individual practitioner toward a system where patients are diagnosed and treated professionally and in accordance with clearly defined protocols. This will help to place checks on the type of treatments and prescriptions that are given out, while also establishing checks and balances that protect both doctors and patients from errors. Having a standardised set of guidelines that must be followed for each condition might seem like a burden but it can help to streamline the process of patient intake and also help even the less experienced doctors perform a thorough examination.
By establishing, following, and updating such protocols we can cut down on medical errors, wrong prescriptions, misdiagnoses and a variety of other medical and clerical errors. This on the whole will make the healthcare industry one that is more geared toward providing the best possible, evidence-based care to patients while also striving to move forward the boundaries of medical research.
WHAT TO DO?
So when it comes to medical decisions that can affect both our health and quality of life we need to be doubly sure about the doctor and the treatment being prescribed. All of us browse dozens of models when it comes to, say buying a laptop or getting a new phone. There's no reason to do otherwise when it comes to expensive and sometimes life-altering medical procedures. Many people think that getting a second opinion is an insult to their GP or family physician, others think that an expensive and elite hospital automatically equals the best care. Most of us know that neither of these is true, the best doctors still have blind spots in their skills and not all hospitals or practitioners are nobly motivated.
Get a second consult: Getting a lateral consult is important and can expose you to alternative methods of treatment. Sometimes between different locations and generations of doctors, the treatment approaches can differ.
Get a Teleconsult: For many of us getting multiple consults from doctors located in different places can be a problem because of the costs involved or due to time constraints, in such cases getting a telemedicine consult can be both a cheap and easy solution. Most insurance providers are starting to cover telemedicine consultations and even paying from your pocket is cheaper as it saves time and effort on both sides.
Talk to others:This doesn't mean talking to random strangers, it means talking to other people undergoing the same treatment or suffering from the same disease. In this age of social media, it is quite easy to find support groups, information groups, and chat rooms for people going through the same disease or condition. In fact, it was through a Facebook group that women who had severe pain and inflammation following the implantation of an IUD contraceptive found each other and learned that the medical IUD manufactured was faulty, eventually, they sued the company and won a lawsuit and most importantly took that defective product off the market so that others would not suffer the same way they did.
All said and done, it is up to the patient and to an equal extent the doctor to ensure that the practice of medicine is about improving the quality of life and treating the disease above all else.