10 things EMS providers need to know about Telehealth
1. UNDERSTAND THE DIFFERENCE BETWEEN TELEHEALTH AND TELEMEDICINE
Telehealth is an all-encompassing concept of delivering healthcare, monitoring and managing healthcare of a patient or population remotely. Telemedicine is a subset of this and is primarily concerned with the delivery of active interventional care to people located remotely.
Telemedicine is dispensing case by case care for current or ongoing medical conditions and often requires the active review or interpretation of a qualified physician or specialist. This can be an important distinction to have in a setting such as Emergency services where care needs to be delivered in an accurate and fast paced manner to save lives. Telemedicine consultations will be taking place while the vehicle is in transit to the nearest hospital or trauma centre and the medical care provided by paramedics can be augmented by a doctor in a remote location.
There are many cases of trauma that can benefit from a live consult with a trauma specialist to help in triage and management of the patient, such expert help in assessing and guiding treatment can significantly increase survival chances and reduce adverse outcomes or long term complications. EMS services are in the business of rapid care and serve only as a stopover between an accident site and the hospital. There are some cases where only the most basic stabilization is possible and the essence of care is transporting them as quickly as possible to a hospital.

2. USING TELEHEALTH APPLICATIONS DOESN’T MEAN YOU DON’T KNOW HOW TO ASSESS A PATIENT
EMT's are highly trained and are regularly exposed to do or die situations that require split second decision making. In that aspect they far outstrip many doctors and nurse practitioners. Paramedics usually deal with the crying, sobbing patient who is in pain, their loved ones who are panicking or they deal with an unconscious patient and unhelpful or hostile bystanders.
The implementation of Telehealth can be seen to be a move that question the capability, competence and skills of the EMS teams but nothing could be further from the truth. The use of Telemedicine is an adjunct to routine care that allows EMS crews to deal with variables and issues in the field flexibly and quickly thanks to assistance from a remote physician. A doctor or specialist can be a valuable resource to an EMS crew as they serve as a fresh set of eyes, a safety net and a rotating member of the crew that they can rely on for spot diagnosis.
Ultimately the goal is to save as many patients as possible and where possible minimize long term complications for them. EMS teams have struggled alone in remote locations and hazardous weather conditions to make this possible but with the inclusion of telemedicine theya re no longer alone in the fight, a virtual roster of doctors are there to assist and support them whenever they are needed.
3. TELEHEALTH BENEFITS EMS PROVIDERS
There are a plethora of benefits to EMS providers with regards to adopting Telehealth.
- Saves time in dispensing care and makes reaction times of ambulance crew better.
- Helps in streamlining the care process.
- Reduced adverse outcomes.
- Reduced long term complications for the patients.
- Specialty care can be provided in transit
- Initiate TPA and clot busters in ambulance with cardiologist oversight.
- Perform stroke assessment with a remote neurologist consult.
- Get a paediatrician consult for neonatal patients.
- Geriatric specialty care for an increasing elderly population.
- Handholding care for transit ambulances shifting patients over long distances.
- Make full use of the golden hour
- Prepare the ER to receive the patient with the right preparations and equipment.
There is often a lag between the time the patient is transferred to a hospital and continuance of medical care, this lag can prove fatal or lead to complications, longer recovery periods etc.
HOW CAN TELEMEDICINE HELP?
Telemedicine is easy and cheap to implement as long as a device with internet connectivity, a doctor at a remote location, secure server are available.
By creating a Teleconsultation with a specialist such as a cardiologist, neurologist or pediatrician the EMS crew can easily overcome gaps in their knowledge and initiate triage or life-saving protocols in the field.
Laws in many countries curtail the level of treatment, medication, or procedures that EMS crews are allowed to perform. The scenario changes however when a qualified medical specialist is supervising said treatment, thus the patient can receive a higher standard of care especially when it comes to remote communities located far away from a medical facility.
EMT personnel can also benefit from the supervision and expertise of a specialist and learn on the job, there is greater potential for lateral transfer of knowledge and they can handle similar emergencies with greater confidence.
Tele-EMS has been successfully piloted in several places around the world, one such example would be the town of Aachen which used TELE-EMS in conjunction with regular emergency services. It was observed that there was a qualitative leap inefficiency and the bandwidth of emergencies that they could attend to.
4. TELEHEALTH PARTICULARLY BENEFITS EMS PROVIDERS IN RURAL AREAS
EMS services face additional burdens in rural areas compared to cities and one of the main reasons can be that there are far fewer private players involved in serving rural communities. Rural EMS care is a separate beast that faces its own set of problems.
- Poor road connectivity
- Poorly maintained infrastructure
- Mountainous or difficult terrain
- Longer transit times to a higher tier medical centre unlike in cities where there is a massive glut of private and public hospitals.
- Lower remuneration
- Need to cover a wider range of complaints and emergencies from animal attacks, poisonings, domestic violence, mass casualties, less common diseases to pregnancy and neonatal emergencies.
- Night time emergencies can be more dangerous due to poor visibility and dangerous roads.
- Environmental obstacles such as heavy rain, snowfall, landslides etc can interrupt services.
- EMS needs to provide longer term care and for a wider range of complaints than usual and this translates into higher training needs, more equipment, longer working hours.
5. TELEHEALTH BENEFITS PATIENTS
For patients including Telemedicine into the care cycle can have tangible benefits especially in terms of EMS. A significant number of EMS calls end up being false alarms because someone mistook a heartburn or gas after a spicy meal for a heart attack, Parents can freak out over minor injuries to their children or small issues and alert EMS services only to end up taking a wasted and quite expensive round trip to the hospital. Every call that is a false flag can take an ambulance and crew away from some other emergency. For patients a Teleconsult that rules out an emergency event can save them a lot of time and money. This is especially true for those with no health insurance or where policies fail to provide coverage for such incidents.
The main benefit for patients is that initiating a teleconsult while in transit with an expert in the required field can increase the odds of their survival and lessen the chances that they will need protracted or invasive treatments. There is also the added advantage that the doctor in the consult can loop in other specialists on the fly to give enhanced care, they can also intimate the hospital to prepare OR's , equipment, call for blood or in the case of severe injuries re route the ambulance to a hospital that is better equipped to handle the case.
6. TELEHEALTH CAN AID IN TIME-SENSITIVE CASES LIKE TRAUMA, STEMI AND STROKE
As a routine paramedics have limited authority to initiate certain types of protocols or increase the dosage of certain drugs without the supervision or instructions of a doctor. This is something they can be fired over and even sued over, as such EMT techs are understandably hesitant to initiate or break certain protocols that can make the difference between life and death in cases such as strokes, cardiac issues, embolisms, trauma and bleeding etc.
In many cases paramedics have limited training in advanced trauma or life support such as placing an intraosseous line and they don't try it. Certain signs and symptoms may be very apparent to a doctor or specialist but can be easily missed by an EMT during a bumpy high speed ambulance ride. Having a Telemedicine consult means that a doctor can look at the situation live, suggest procedures, guide the EMT's, authorize higher doses, start anti platelet therapy, clot busting procedure, cardiac care etc inside the ambulance.
This handholding can be a great learning experience for EMS crews as well and they are more likely to similar emergencies with greater confidence. A lateral and top down transfer of skills and knowledge can occur that boosts the performance of the field as a whole.
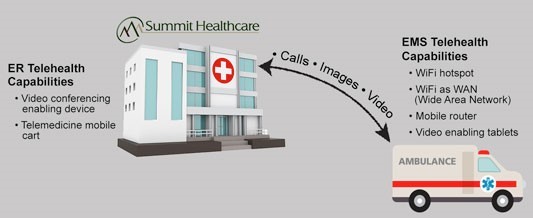
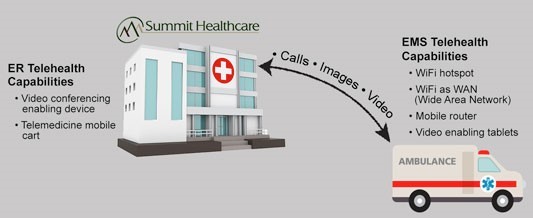
7. NO COMPLEX INFRASTRUCTURE IS NEEDED TO MAKE TELEHEALTH WORK RELIABLY
Telehealth software can work reliably with just the bare minimum in terms of requirements or investments. Most telemedicine software can work on standard devices that are either connected to the internet or not. Preloaded forms, fields to record vitals, emergency work flows can be built in to maximize the time available for the consult.
Using Peripheral devices that directly send data to the telemedicine application can save time and effectively use the golden hour for EMS paramedics and techs. The door to needle time can be made zero. These battery operated devices that can send data over Bluetooth or WIFI can save time and doctors at the hospital can monitor a patient's vitals in real-time even as they are on route to the trauma bay and intervene as necessary. This saves valuable time during the handoff of the patient by EMS crews as the receiving nurses/doctors are kept up to date on the patient's vitals and condition.
The installation, infrastructure costs of adding a few devices, screen/tab and telemedicine software to an ambulance is only a drop in the bucket compared to annual functioning and maintenance charges usually faced by EMS providers.
8. DO YOUR RESEARCH AND FIND OUT WHAT PLATFORMS ARE AVAILABLE AND BEST FOR YOUR AGENCY
Although telehealth can work on most any hardware, you need to find the applications that best meet your agency’s needs and goals. For example, CureSelect Healthcare allows communication outside of just one organization.
There are a lot of other companies that might do HIPAA-compliant messaging and texting securely for their patient, and they do it well, However, they only do it within their hospital system. Porting medical records and data or looping in others during the consult is not a facility available on many telemedicine platforms.
Tele-EMS software crosses organizations and can be done simply and quickly, and as a case evolves, the app allows you to add people to the conversation.
“It’s intuitive and available, with the ability to use whatever hardware you have with these smartphones connected to cell service or WiFi, and then a platform that allows you to connect securely,” “And you can communicate how you want, whether that’s texting, images, video, alerts or messaging.”
9. YOU CAN DO TELEHEALTH AND STILL MAINTAIN HIPAA COMPLIANCE
HIPAA compliance and data security is the foremost concern with Telehealth and is also the most often stated drawback. While patient data, medical records and video consults are all proprietary personal data that should never be leaked, hackers and ransomware threats are increasingly targeting them. This data can be sold to drug companies, insurance companies, held for ransom especially data regarding STI's or HIV, all of this has greatly alarmed the medical community and patients in particular.
To combat this even stricter data security guidelines have been imposed by both national and international regulatory bodies on any software that deals with sensitive patient information. HIPAA compliance, SOC 2, AES 256, mandatory remotely located secure cloud servers etc have all been made the standard for the industry. EMS Telehealth software can be equipped with all these data security protocols and can thus be deployed with minimal issues.
IN CONCLUSION
Telehealth solutions have been tried in isolated pockets or as pilot programs and they have qualitatively improved EMS services. A program done in Aachen showed remarkable improvements in survival rates, response times and flexible response to various scenarios. Telehealth is here to stay and its permeation into the medical field will only increase with the rapid growth of technology. With the rollout of 5G, faster internet, faster computing systems and AI based intuitive software Telehealth in EMS can be not just an assistive tool but also a predictive and analytical one.