How Tele EMS can help a broken system
Telehealth has become a vital part of healthcare in today's world. One of the many applications that Telehealth and Telemedicine have been recently applied to the field of EMS (Emergency Medical Services). In any medical scenario one of the key fields of medicine is emergency medical services.
Emergency medicine is a cornerstone of the field of health care and is often the starting point for a care cycle that ultimately ends in the ICU or Operating theatre. Accidents, trauma, evacuations, heat stroke, exposure, burns, you name it and the condition can be seen as a routine in emergency services. As such paramedics and EMT's have to be highly trained in a wide range of medical conditions, interventions, counselling, triage etc. But more often than not in countries like India the EMT training programs are far from robust.
CHALLENGES
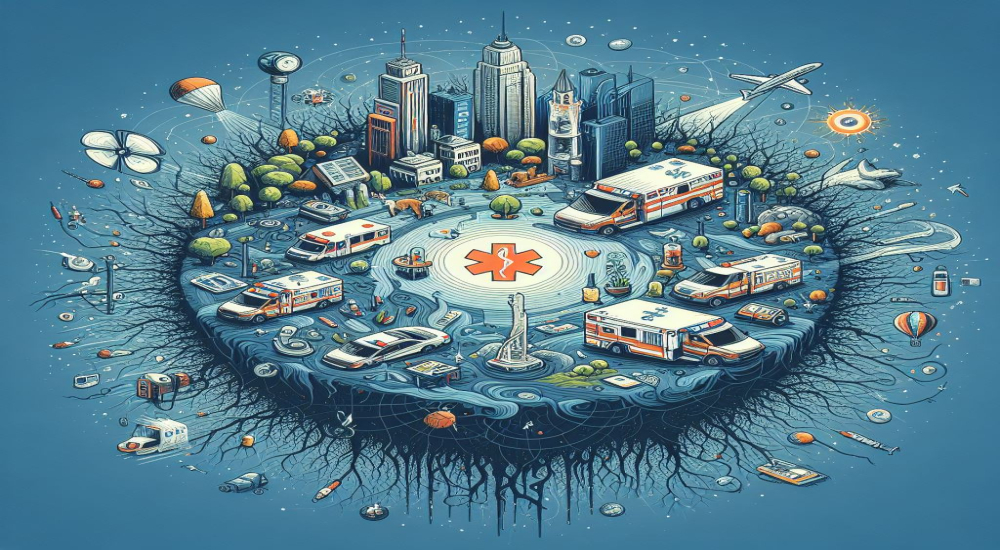
India is a country with a vast, growing population and in a healthcare system such as the one it has EMS plays a vital role in healthcare delivery. EMS services provide medical services not just in the event of accidents, trauma, and cities but also on highways, rural areas, and across state borders.
India has one of the largest road networks in the world and has the number of accidents to match it as well. State governments as well as the NHAI depend heavily on road ambulances to help victims and get them to nearby hospitals. It is only in recent years that a coordinated multi-agency network to deal with emergencies has been piloted. In fact, there is no single ambulance call number across the country. Many states have adopted the 108 models that was pioneered by Tamil Nadu (adopted by 7 other states, North Indian states have their own EMS call numbers such as 105, 107, etc).
With such nascent steps and few regulations in place more often than not EMT crews are not well trained or well equipped to deal with a variety of emergencies and this can prove fatal to victims when their first point of medical contact is not thoroughly trained or vetted.
By law ambulances in India are required to transport patients to the nearest available government hospital or medical facility and in the absence of the same, they are to take the patient to the nearest medical center for treatment. However, the ground reality is that there is a huge mix of private and public ambulances plying the road especially in cosmopolitan cities such as Chennai, Bangalore, Mumbai, etc and they prioritize transport to their own hospitals in violation of this protocol.
Several cases of bribery and corruption have been documented in ambulance service providers where drivers accept bribes from private hospitals and transport patients to those hospitals rather than the nearest government center. This proves both financially expensive for patients who may not be able to afford care and also adversely affects the outcome for severely injured patients.
DECLINING STANDARD OF CARE
There is no unified standardization that is applied across all states and union territories in India, this makes it hard to assess the performance, enforce regulations and create good operating standards. Paramedics, ambulance drivers, and EMTs abroad have mandatory examinations, yearly assessments, special courses for high-speed driving and safety, equipment check, audits, and inspections. All of these are sorely lacking in India.
Most paramedics in India have unrelated educational qualifications, receive minimal training, and are poorly supervised. Many may be high school dropouts with very little knowledge about various medical emergencies and their handling protocols. For many, the ambulance service functions merely as a transportation vehicle and not as the first line of treatment to stabilize a patient.
The large influx of private ambulances in the country has led to any vehicle with four wheels and some space being converted into an ambulance, during the COVID pandemic vans meant for personal use were jerry-rigged to work as ambulances. These are glorified Uber's for patients and don't live up to the global standards for ambulances including equipment, personnel, and medicines. This means that patients often end up with long-term complications that could have been avoided if the early intervention had been initiated in the ambulance.
Some medical emergencies such as Strokes, Cardiovascular events, and neonatal emergencies benefit greatly from early staging and initiation of treatment. A classic example is the initiation of Stroke Protocol by EMTs and administration of TPA ( tissue plasminogen activator) en route to the hospital, this greatly improves the outcome for stroke patients and significantly shortens their recovery time and extent of debilitating events.
WHAT WE NEED
India is a country with a diverse population with people from every social and economic stratum vying for medical services. A common point of access for every age, gender, and strata would be emergency services and as such, there is a veritable cornucopia of reasons an EMS call can be initiated.
In such a scenario what we need most of all is quick, timely, efficient, and effective care delivered by our EMS services. To do that well need to up the ante and take some steps, implement programs with a long view in mind.
- Nation-wide standardization for ambulance vehicles.
- Mandatory equipment lists and medication lists for every ambulance.
- Minimum training and qualifications standard for paramedics.
- Regular review courses and mandatory re-certification programs.
- Strict enforcement of codes and penalties for infractions by both individuals and ambulance operators.
HOW CAN TELEMEDICINE HELP?
Telemedicine is easy and cheap to implement as long as a device with internet connectivity, a doctor at a remote location, secure server are available.
By creating a Teleconsultation with a specialist such as a cardiologist, neurologist or pediatrician the EMS crew can easily overcome gaps in their knowledge and initiate triage or life-saving protocols in the field.
Laws in many countries curtail the level of treatment, medication, or procedures that EMS crews are allowed to perform. The scenario changes however when a qualified medical specialist is supervising said treatment, thus the patient can receive a higher standard of care especially when it comes to remote communities located far away from a medical facility.
EMT personnel can also benefit from the supervision and expertise of a specialist and learn on the job, there is greater potential for lateral transfer of knowledge and they can handle similar emergencies with greater confidence.
Tele-EMS has been successfully piloted in several places around the world, one such example would be the town of Aachen which used TELE-EMS in conjunction with regular emergency services. It was observed that there was a qualitative leap inefficiency and the bandwidth of emergencies that they could attend to.
POTENTIAL DRAWBACKS
There is a propensity for EMT especially highly trained veterans in the field to resist change. The commonly faced hesitancy can be due to one of the following reasons.
- Fear of using technology especially unfamiliar new software and work flows.
- The feeling that their competency or skills are being questioned by using Telemedicine.
- Difficulty in adapting to new procedures and workflows.
- Fear of increased paperwork, liabilities or using the new equipment required for teleconsultations.
- Many older paramedics and doctors are not tech-savvy and they are hesitant to implement such changes.
- There can be an interruption to the regular workflows.
- Connectivity issues, and doubts about the frequency or effectiveness of use can be an issue.
- Connecting with doctors from different states or medical boards can cause legal issues.
A FORCE FOR THE GREATER GOOD
Tele-EMS systems can be easily integrated with location tracking, fuel consumption trackers, maps, and guides to the shortest routes with live traffic updates with the use of simple tech and google maps plugins. This can save time and effort for the patients and ambulance personnel by optimal time utilization. Both government-owned and private aggregators for ambulances can track crew locations, time to pick up the patient, time for drop off, etc to streamline their process. Plenty of governments at state and local levels can use such data collected by Telemedicine software to make policy changes.
The idling time of each vehicle, whether they comply with laws and go to the nearest hospital, keeping track of medications given during the ride, using Teleconsultations for emergency management and initiating treatment, and increasing the overall standard of EMS services care is possible with a Telehealth software to connect. Telemedicine is not limited by distance and can be applied to both air ambulances, live Teleconsult during Medevacs, Hospital ships, and sea ambulances, etc.