Revolutionizing Stroke Care: The Role of Telemedicine in Saving Lives
In the realm of emergency medicine, every second counts, especially when it comes to stroke care. Time is of the essence in treating strokes, as delays can lead to irreversible brain damage or even death. However, with the advent of telemedicine, a new era of stroke care has emerged, one that holds the promise of significantly improving patient outcomes and survival rates.
Telemedicine, the use of telecommunications technology to provide healthcare remotely, is transforming the way stroke patients are treated, particularly in the critical pre-hospital and emergency room phases. By seamlessly connecting ambulances, emergency medical technicians (EMTs), neurologists, and the emergency room, telemedicine is revolutionizing the delivery of stroke care in several key ways:
- Early Assessment and Diagnosis: Time is brain when it comes to strokes. With telemedicine-enabled ambulances equipped with mobile telestroke units, EMTs can quickly assess patients suspected of having a stroke using video conferencing technology. This allows neurologists to remotely evaluate the patient's symptoms, conduct neurological assessments, and make timely treatment decisions even before the patient arrives at the hospital.
- Streamlined Communication: Telemedicine facilitates real-time communication and collaboration between EMTs, neurologists, and emergency room staff. Through secure video conferencing and electronic medical record systems, healthcare providers can share vital patient information, such as medical history, imaging results, and vital signs, ensuring a smooth transition of care and eliminating delays in treatment.
- Expert Consultation: Telemedicine enables remote neurologists to provide expert consultation to emergency room physicians, guiding them in the administration of time-sensitive treatments such as thrombolytic therapy (clot-busting drugs) or endovascular procedures (mechanical clot removal). This access to specialized expertise ensures that stroke patients receive the most appropriate and effective interventions based on the latest evidence-based guidelines.
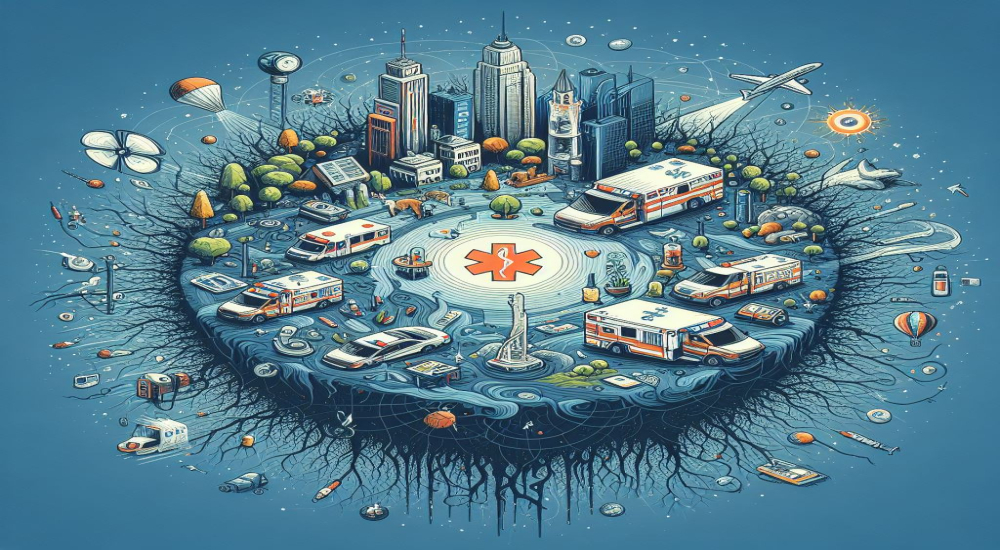
- Improved Access to Care: Telemedicine breaks down geographical barriers and enhances access to specialized stroke care, particularly in underserved rural areas where neurologists may be scarce. By leveraging telemedicine technology, rural hospitals can connect with stroke centers and neurology experts, enabling timely diagnosis and treatment for patients who might otherwise face significant delays in care.
- Post-Stroke Care and Rehabilitation: Telemedicine extends beyond the acute phase of stroke care, offering remote monitoring and follow-up consultations for stroke survivors during their recovery and rehabilitation. Virtual rehabilitation programs, teletherapy sessions, and remote monitoring of vital signs and medication adherence empower patients to actively participate in their recovery journey while receiving ongoing support from healthcare providers.
By integrating telemedicine into the stroke care continuum, healthcare systems can achieve several crucial goals: reducing treatment delays, minimizing disability and mortality rates, improving patient satisfaction, and optimizing resource utilization. However, widespread adoption of telestroke programs requires investment in technology infrastructure, training for healthcare professionals, reimbursement policies that support telemedicine services, and ongoing quality improvement initiatives.
In the realm of emergency medicine, time is of the essence. Every second counts, especially when it comes to critical conditions like strokes where prompt treatment can be the difference between life and death, or between full recovery and lasting disability. In recent years, the integration of telemedicine into ambulance services has emerged as a groundbreaking approach to enhancing the efficiency and effectiveness of emergency response, particularly in the context of stroke management.
The Challenge of Stroke Response
Stroke, often referred to as a "brain attack," occurs when blood flow to the brain is interrupted or reduced, leading to the deprivation of oxygen and nutrients to brain tissue. This medical emergency requires swift intervention to minimize brain damage and optimize patient outcomes. However, diagnosing and treating strokes in the field present significant challenges for Emergency Medical Technicians (EMTs) and paramedics.
Traditionally, EMTs rely on their clinical expertise and limited diagnostic tools to assess patients suspected of having a stroke. Time is lost during transport to the hospital, where confirmation of diagnosis and initiation of treatment can be delayed further. In such critical situations, every minute wasted increases the risk of irreversible neurological damage.
The Role of Telemedicine in Ambulances
Telemedicine, the remote diagnosis and treatment of patients via telecommunications technology, offers a transformative solution to these challenges. By integrating telemedicine capabilities directly into ambulances, emergency responders can connect with remote medical professionals in real-time, enabling rapid assessment, diagnosis, and treatment initiation even before arrival at the hospital.
Here's how telemedicine can be deployed effectively in ambulances for stroke response:
- Remote Consultation: When a patient is suspected of having a stroke, EMTs can initiate a telemedicine consultation with a neurologist or stroke specialist. Through live video conferencing, the remote doctor can visually assess the patient, review vital signs, and gather pertinent medical history from both the patient and the on-site EMTs.
- Diagnostic Support: Telemedicine platforms can integrate tools for remote diagnostic testing, such as portable electrocardiograms (EKGs) and mobile imaging devices. These tools allow the remote physician to conduct real-time assessments, including the interpretation of EKGs and rapid imaging studies like computed tomography (CT) scans or magnetic resonance imaging (MRI) to confirm the stroke diagnosis.
- Treatment Guidance: Once the diagnosis is confirmed, the remote physician can provide guidance on appropriate treatment protocols, including the administration of clot-busting medications like tissue plasminogen activator (tPA) or arranging for transfer to a Comprehensive Stroke Center for endovascular therapy. This real-time decision support can significantly reduce the time to treatment initiation, improving patient outcomes.
- Continuous Monitoring: Throughout the transport process, the telemedicine system allows for continuous monitoring of the patient's condition, enabling the remote physician to adjust treatment strategies as needed and anticipate any complications that may arise en route to the hospital.
Benefits of Telemedicine in Ambulances for Stroke Response
The integration of telemedicine into ambulance services offers several benefits for stroke management:
- Faster Treatment Initiation: By facilitating early diagnosis and treatment initiation in the field, telemedicine helps minimize the delay in critical interventions, reducing the risk of permanent brain damage.
- Enhanced Accuracy: Remote consultation allows for access to specialized expertise and diagnostic tools that may not be available on-site, improving the accuracy of diagnosis and treatment decisions.
- Improved Outcomes: Timely access to appropriate stroke care has been shown to improve patient outcomes, including reduced disability and mortality rates.
- Optimized Resource Utilization: Telemedicine enables more efficient utilization of healthcare resources by streamlining the triage process and ensuring that patients are directed to the most appropriate level of care based on their condition.
Challenges and Considerations
While the integration of telemedicine into ambulance services holds great promise for improving stroke care, several challenges must be addressed:
- Technological Infrastructure: Ambulance telemedicine systems require robust telecommunications infrastructure to ensure reliable connectivity, particularly in remote or rural areas where internet access may be limited.
- Training and Education: EMTs and paramedics need adequate training to effectively use telemedicine technology and interpret remote physician guidance. Ongoing education and support are essential to ensure proficiency and confidence in using these systems.
- Regulatory and Reimbursement Issues: Regulatory frameworks and reimbursement policies may need to be adapted to support the widespread implementation of ambulance telemedicine programs, including licensure requirements for remote physicians and reimbursement for telemedicine consultations.
- The integration of telemedicine into ambulance services represents a paradigm shift in emergency medicine, empowering EMTs and paramedics with the resources and expertise needed to deliver timely and effective care to patients experiencing acute medical emergencies like strokes. By leveraging telecommunications technology to connect with remote physicians, ambulance telemedicine programs have the potential to revolutionize stroke response, ultimately saving lives and improving patient outcomes. As technology continues to evolve and healthcare systems adapt to embrace innovation, the future of emergency care looks brighter than ever before.
- In conclusion, telemedicine holds tremendous potential to revolutionize stroke care by bridging the gap between pre-hospital, emergency, and post-stroke settings. By harnessing the power of telecommunications technology, we can transform the way strokes are diagnosed, treated, and managed, ultimately saving lives and improving the quality of life for stroke survivors. As we continue to innovate and integrate telemedicine into stroke care protocols, we move closer to achieving the goal of providing every stroke patient with timely and effective treatment, regardless of their location or circumstances.